BOSTON — Many new treatments for cancer cost nearly $100,000 a year, sparking fresh debate about how much a few months more of life is worth.
The latest is Provenge, a first-of-a-kind therapy approved in April. At $93,000 a year, it adds four months’ survival, on average, for men with incurable prostate tumors. Bob Svensson is honest about why he got it: insurance paid.
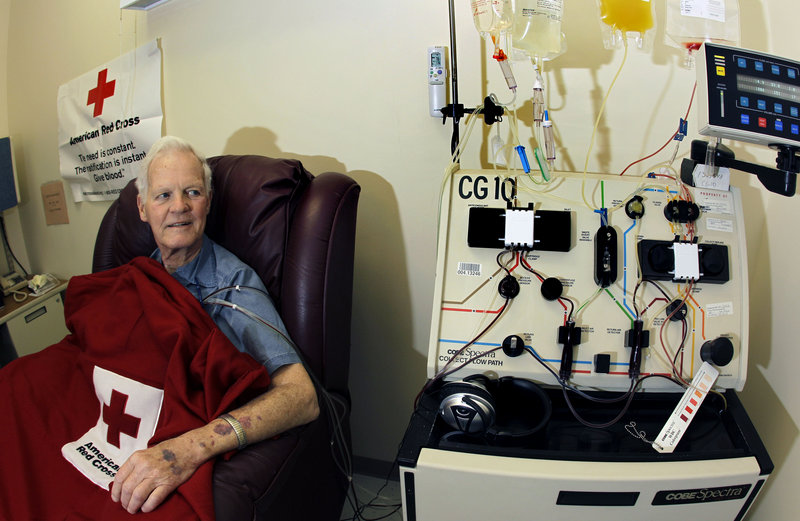
“I would not spend that money,” because the benefit doesn’t seem worth it, says Svensson, 80, a former corporate finance officer from Bedford, Mass.
His supplemental Medicare plan is paying while the government decides whether basic Medicare will cover Provenge and for whom. The tab for taxpayers could be huge — prostate is the most common cancer in American men. Most of those who have it will be eligible for Medicare, and Provenge will be an option for many late-stage cases. A meeting to consider Medicare coverage is set for Nov. 17.
“I don’t know how they’re going to deal with that kind of issue,” said Svensson, who was treated at the Lahey Clinic Medical Center in suburban Boston. “I feel very lucky.”
For the last decade, new cancer-fighting drugs have been topping $5,000 a month. Only a few of these keep cancer in remission so long that they are, in effect, cures. Insurers usually pay if Medicare pays. But some people have lifetime caps and more people are uninsured because of layoffs in the recession. A new federal law eliminates these lifetime limits for plans that were issued or renewed on Sept. 23 or later.
Celgene Corp.’s Revlimid pill for multiple myeloma, a type of blood cancer, can run up to $10,000 a month; so can Genentech’s Avastin for certain cancers. Now Dendreon Corp.’s Provenge rockets price into a new orbit.
Unlike drugs that people can try for a month or two and keep using only if they keep responding, Provenge is an all-or-nothing $93,000 gamble. It’s a one-time treatment to train the immune system to fight prostate tumors, the first so-called cancer vaccine. Part of why it costs so much is that it’s not a pill cranked out in a lab, but a treatment that is individually prepared, using each patient’s cells and a protein found on most prostate cancer cells.
It’s also in short supply. At the University of Texas M.D. Anderson Cancer Center, doctors plan a lottery to decide which of its 150 or so eligible patients will be among the two a month it can treat with Provenge. An insurance pre-check is part of the process to ensure they financially qualify for treatment.
“I’m fearful that this will become a drug for people with more resources and less available for people with less resources,” said M.D. Anderson’s prostate cancer research chief, Dr. Christopher Logothetis.
For other patients on other drugs, money already is affecting care:
• Job losses have led some people to stop taking Gleevec, a $4,500-a-month drug that keeps certain leukemias and stomach cancers in remission. Three such cases were recently described in the New England Journal of Medicine. All those patients suffered relapses.
• Retirements are being delayed to preserve insurance coverage of cancer drugs. Holly Reid, 58, a Novato, Calif., accountant, hoped to retire early until she tried cutting back on Gleevec and her cancer recurred. “I’m convinced now I have to take this drug for the rest of my life” and will have to work until she’s eligible for Medicare, she said.
• Lifetime caps on insurance benefits are hitting many patients, and laws are being pushed in dozens of states to get wider coverage of cancer drugs. In Quincy, Mass., graduate student Thea Showstack, 30, testified for one such law after pharmacists said her first cancer prescription exceeded her student insurance limit. “They said, ‘OK, that will be $1,900,’” she said. The federal health care law forbids such caps on plans issued or renewed Sept. 23 or later.
Doctors also have questioned the value of Genentech’s Tarceva for pancreatic cancer. The $4,000-a-month drug won approval by boosting median survival by a mere 12 days. Here’s how to think about this cost: People who added Tarceva to standard chemotherapy lived nearly 6.5 months, versus six months for those on chemo alone. So the people taking Tarceva spent more than $24,000 to get those extra 12 days.
When is a drug seen as cost-effective?
The most widely quoted figure is $50,000 for a year of life, “though it has been that for decades — never really adjusted — and not written in stone,” said Dr. Harlan Krumholz, a Yale University expert on health care costs.
Many cancer drugs are way over that mark. Estimates of the cost of a year of life gained for lung cancer patients on Erbitux range from $300,000 to as much as $800,000, said Dr. Len Lichtenfeld, the American Cancer Society’s deputy chief medical officer.
There’s no rule on how much is too much for a medical treatment, he said.
Insurers usually are the ones to decide, and they typically pay if Medicare pays. Medicare usually pays if the federal Food and Drug Administration has approved the use.
If people lose insurance coverage, they often discover they can’t afford their medicines, said Dr. Alan Venook, a University of California, San Francisco cancer specialist. He wrote in the New England Journal in August about three of his patients who stopped taking or cut back on Gleevec because of economic hardship.
Two of the three now get Gleevec from its maker, Novartis AG, which like most drug companies has a program for low-income patients. About 5,000 patients got help for Gleevec last year, said Novartis spokesman Geoffrey Cook.
Showstack gets Gleevec from Novartis. The dose she’s on now would cost $50,000 a year.
“I’m not actually sure that I know anyone who could afford it,” she said.
Gleevec’s cost is easier to justify, many say, because it keeps people alive indefinitely. About 2,300 Americans died each year of Showstack’s form of leukemia before Gleevec came on the market; only 470 did last year.
“I don’t think we quibble with a drug that buys people magical quality of life for years,” Venook said.
It’s unclear whether Provenge will ever do that — it needs to be tested in men with earlier stages of prostate cancer, doctors say. So far, it has been tried and approved only for men with incurable disease who have stopped responding to hormone therapy. On average, it gave them four months more, though for some it extended survival by a year or more.
Until it shows wider promise, enthusiasm will be tepid, said Dr. Elizabeth Plimack, a prostate specialist at the Fox Chase Cancer Center in Philadelphia.
“I’ve not had any patient ask for it,” she said.
Logothetis, at M.D. Anderson, said Provenge and other cancer vaccines in development need “a national investment” to sort out their potential, starting with Medicare coverage.
“It’s no longer a fringe science. This is working,” he said. “We need to get it in the door so we can evolve it.”
Send questions/comments to the editors.


Success. Please wait for the page to reload. If the page does not reload within 5 seconds, please refresh the page.
Enter your email and password to access comments.
Hi, to comment on stories you must . This profile is in addition to your subscription and website login.
Already have a commenting profile? .
Invalid username/password.
Please check your email to confirm and complete your registration.
Only subscribers are eligible to post comments. Please subscribe or login first for digital access. Here’s why.
Use the form below to reset your password. When you've submitted your account email, we will send an email with a reset code.