WASHINGTON –Buried in the $16.3 billion Veterans Affairs bill that President Obama signed into law Thursday are provisions for greater department transparency, such as a mandated 90-day report on wait times at each VA hospital, and a six-month report that would include health statistics and measurements of patient quality at all facilities.
Much of this data was made public two months ago, after the Department of Veterans Affairs responded to the public outcry over patient delays and falsified appointment records at some veterans facilities.
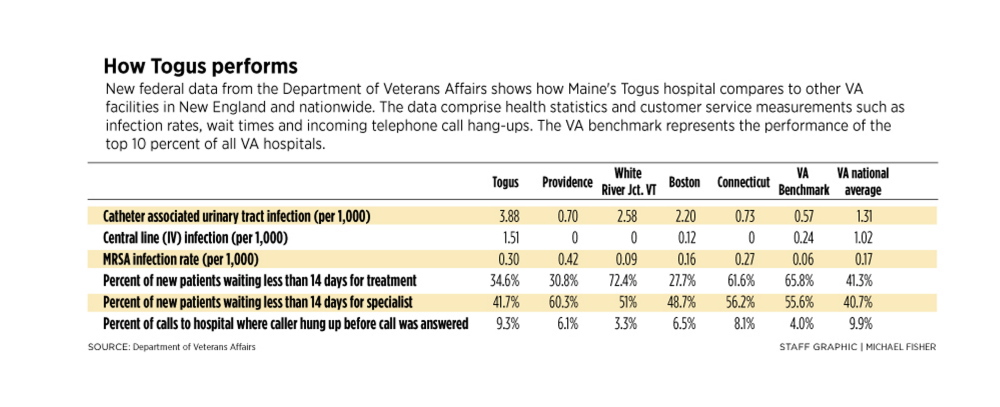
Since the controversy began, Maine’s VA health care system has notably stood apart for its unadulterated scheduling and shorter wait times. But the recently released data on a broad variety of health statistics measuring deaths, avoidable events and customer satisfaction paint a far more complex picture beyond making appointments.
The data, collected internally by the VA, show that among New England VA hospitals, Maine’s had the highest rate of catheter-associated urinary tract infections, the highest rate of IV-associated blood infections, and the second highest rate of infections for Methicillin-resistant Staphylococcus aureus, or MRSA, a staph bacterium that is resistant to antibiotics.
The Maine VA Medical Center at Togus in Augusta also had the region’s second-highest 30-day death rate and the second-highest estimated 30-day death rate due to pneumonia.
While the data offer a more in-depth look at performance measurements, officials caution about drawing definitive conclusions without understanding the circumstances of each hospital, such as patient mix and their complexity levels.
“The report is an important measure but it is best utilized as a proactive tool for probing deeper, to help identify any issues that arise, not for making conclusions across sites,” said Ryan Lilly, center director for the VA Maine Healthcare System, which treated 40,000 acute-care patients at Togus over the last fiscal year.
The source of the data is an internal online reporting tool known as Strategic Analytics for Improvement and Learning, or SAIL, which was developed to give top VA brass a quick snapshot view of all 147 VA medical centers. The internal version includes a one- to five-star scoring system for each hospital.
The VA released a summary of 2013 SAIL data in June, less than a week after The Wall Street Journal reported that VA hospitals across the country showed disparate treatment.
The Journal cited leaked SAIL data for Boston’s VA hospital that it scored five out of five stars, while the Phoenix VA hospital received one star. The agency said in a statement that the stars were not released in the public version because SAIL is best used to compare individual metrics. However, Lilly revealed that Maine’s VA hospital received three stars in 2013.
Even internally, VA officials have disagreed over the use of SAIL’s star scoring system, said Stephan Fihn, director of analytics and business intelligence for the Veterans Health Administration. The ratings were determined by adding all the areas that SAIL measures into a composite score, which erroneously assumes that each measurement is of equal importance, he said.
The star ratings also make it difficult to compare VA hospitals with private hospitals that aren’t rated by stars, Fihn added. A one-star VA hospital might actually be equal to what some may consider a well-performing hospital in the community, Fihn said.
“We thought people would misinterpret the stars rather than look at the individual data,” Fihn said. “The VA has erred on the side of being transparent and putting the data out and we hope that thoughtful individuals will spend the time to try to understand the complexity.”
INFECTION RATES
The released data show that while the Maine VA hospital performed close to the national average in many areas, it scored below other New England VA hospitals and the national benchmark of top-performing VA hospitals in certain measurements.
The VA data do not include raw values that specify the actual numbers of certain types of infections. Instead, it expresses the data in terms of a rate.
For example, Togus’ rate of catheter-associated urinary tract infections was 3.9 – the highest in the region and among the highest rates in the country. This means that for every 1,000 days that patients were on catheters, about four contracted a urinary tract infection at Togus, about seven times the national VA benchmark of 0.57.
A urinary catheter is a tube placed in the body to drain and collect urine from the bladder. Catheters are used during and after some types of surgery and for medical conditions that affect a person’s ability to urinate.
The hospital’s rate for central line, or IV, infections was also the highest in New England, at 1.5 for every 1,000 days patients were on IVs. This was significantly higher than the VA benchmark of 0.24, and higher than the national average rate of 1.
The Maine VA hospital also had the second-highest rate of MRSA in the region. In 2013, for every 1,000 days that patients were in hospital beds, 0.30 patients at Togus contracted MRSA, while he national benchmark was 0.06, and the national average was 0.17.
Togus director Lilly said one reason infection rates are higher in Maine is that the hospital lacks a unit for long-term patients on ventilators. These patients are treated in the acute care unit, and they are often more susceptible to infection, he said.
The SAIL data only counts infections that occur in acute (short-term) care and intensive care units, Lilly said. Larger VA facilities with long-term ventilator units might not include these infections as part of their reporting, while Togus does, he added.
Since October 2013, the hospital has seen a significant drop in infections, Lilly said. It’s been more than six months since Togus has had a single catheter-associated urinary tract infection and more than six months since the hospital saw a MRSA infection in acute care, he said.
Private facilities also struggle with hospital-acquired infections, said Lisa McGiffert, director of the Safe Patient Project at Consumers Union, a national policy and advocacy organization.
“A lot of private hospitals have only recently started to look at catheter-associated UTIs,” McGiffert said. “We’re seeing UTIs coming down a tiny bit, but there are no real reductions yet.”
For a basic private sector comparison, the MaineGeneral Medical Center in Augusta reported 10 catheter-associated urinary tract infections over 2,505 days that patients were on catheters, according to Medicaid.gov. Using the VA’s method of calculating infections per 1,000 days, MaineGeneral had an infection rate of 4. Meanwhile, Eastern Maine Medical Center in Bangor reported 21 infections over 9,458 days, with a rate of 2.2.
It’s important to note that the Medicaid data for private hospitals are limited to infections in intensive care units only and not all the infections that happen in acute care, said Linda Greene, manager of infection prevention at the University of Rochester’s Highland Hospital. Green is also a member of the regulatory review panel of the Association for Professionals in Infection Control and Epidemiology.
However, McGiffert said that generally it appears that catheter-associated urinary tract infections are a problem statewide. Medicaid has a different method of calculating infection rates, but both MaineGeneral and Eastern Maine Medical Center had urinary-tract infection measurements higher than the national benchmark for private facilities.
“What I would say about the VA in Maine is that they’re in line with private hospitals in the area, which isn’t necessarily a good thing,” McGiffert said. “It looks like things are pretty bad in Maine in general. I’ve never pulled three hospitals randomly and had them all worse than their benchmarks.”
DEATH RATES
The SAIL data also show that Maine’s VA hospital had the second-highest estimated 30-day death rate in the region in 2013 – with a rate of 1.1.
This figure estimates the number of patients who died within 30 days of hospital admission, regardless of whether they were still hospitalized or discharged. When the number of expected deaths is equal to the number of actual deaths, the rate is 1. While the 30-day death rate at Togus was only slightly more than expected, it was higher than VA benchmark of 0.78.
Facilities that have a rate greater than 1 are encouraged to more closely examine the records of individual patients to determine whether gaps in care or other factors such as coding may be affecting their aggregate results, said Fihn, of the VHA.
The Maine VA hospital also had the region’s second-highest percent of estimated deaths due to pneumonia at 9.4 percent, behind the Providence VA hospital’s 9.8 percent.
The death rate data are risk-adjusted to take into consideration patients’ genders, ages and what diagnosed diseases they have when admitted, so the statistics aren’t skewed against VA hospitals that see sicker patients.
However, despite efforts to create a fair comparison among all VA facilities, it’s not a perfect science, said Joseph Francis, director of clinical analytics and reporting for the VHA. Differences such as diet, lifestyle, smoking habits, the type of patients that visit a hospital, whether a hospital is in an urban or rural setting and even socioeconomic backgrounds can affect the data, he said.
Lilly added that smaller facilities like Maine’s have a lower patient volume compared to larger urban hospitals, which can disproportionately affect statistics. While Togus had more than 40,000 acute patients in the last fiscal year, White River Junction in Vermont had about 25,000 patients and the Boston VA saw more than 68,000 patients.
Even in the private sector, it can take only one or two incidents at smaller hospitals to significantly affect rates, said the University of Rochester’s Greene.
However, these numbers aren’t meaningless, McGiffert said.
“I get that a major trauma center and a rural hospital are different, but these are veterans with similar problems all over the country,” McGiffert said. “I would be surprised if the veteran population in Maine was significantly different from the population in Vermont or Massachusetts. And Boston sees more patients, so it should be even more of a challenge to keep infections down and yet they have lower rates.”
The best characteristic of the SAIL data is that the benchmarks are set so high – and that the VA has the ability to institute directives to address concerns like hospital-acquired infections – she said.
“What you’re seeing is much richer information about what’s going on. In the private sector we’re just starting to get this,” McGiffert said.
“The data tells me Maine VA needs to do more work. The benchmarks are based on the best VA hospitals in the country, so we know it’s achievable.”
Lisa Chiu can be contacted at:
Lschiu@hotmail.com
Send questions/comments to the editors.


Success. Please wait for the page to reload. If the page does not reload within 5 seconds, please refresh the page.
Enter your email and password to access comments.
Hi, to comment on stories you must . This profile is in addition to your subscription and website login.
Already have a commenting profile? .
Invalid username/password.
Please check your email to confirm and complete your registration.
Only subscribers are eligible to post comments. Please subscribe or login first for digital access. Here’s why.
Use the form below to reset your password. When you've submitted your account email, we will send an email with a reset code.