WASHINGTON — The Trump administration is proposing to rewrite rules on federal payments to hospitals treating older Americans on Medicare, making it easier for patients to see the prices of procedures and care.
As part of annual updates to Medicare payment rules, federal health officials also want to add $1.5 billion for the coming year to the funds for so-called disproportionate share payments that help buffer hospitals from the expense of treating patients who cannot pay their bills. The increase is a sign that government expects an influx in uninsured patients – something administration officials seldom discuss amid their policies to weaken the Affordable Care Act.
In addition, the revisions seek to motivate hospitals to improve electronic medical records, while eliminating certain measures of the quality of care that the government now requires them to report.
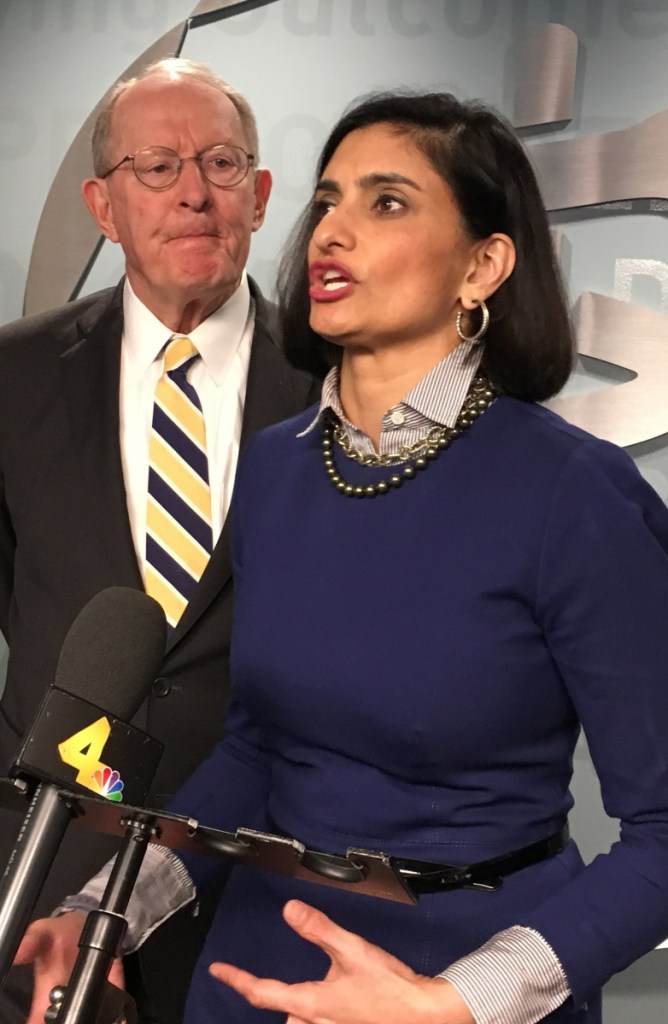
In a conference call with reporters on Tuesday, the administrator of the Centers for Medicare and Medicaid Services portrayed the payment changes her agency is recommending as part of a broad policy to “put patients first.” Seema Verma said the goal is to move away from a system that reimburses hospitals for the number of services they provide to one that rewards them for the value of their care.
The nearly 1,900-page proposed rule calls on hospitals to publish their standard charges online in a machine-readable form that will help insurers and other organizations analyze them. Verma said that would improve the transparency of hospital prices, empowering patients to choose where to go for treatment.
One health-policy expert said that posting prices, while useful, is not as significant as insurance companies helping patients understand what portion of a hospital’s charges they would need to pay themselves.
Another aspect of the proposal would revamp the federal program that encourages hospitals to improve electronic health records, requiring them to share the data in a form that patients can take to their doctors or other health-care facilities.
Starting in 2019, hospitals’ federal ratings would be heavily influenced by whether they provide health records in this manner, which is known as interoperability. Those that do not would be at risk of penalties in their Medicare payments starting two years later, according to a CMS official who spoke to reporters on the condition of anonymity.
The proposed rule also incorporates President Trump’s goal – first broached in an executive order he signed the night he was sworn into office – to reduce the burden the government places on parts of the health-care system. The rule would eliminate 19 measures of quality that hospitals are required to report and get rid of what officials said is duplication in 21 others.
Verma said the idea is to preserve “only those measures that are meaningful in improving patient care,” while dropping ones that are too burdensome to report or ones with which virtually all hospitals already comply.
The changes would apply to about 3,330 acute-care hospitals and more than 400 long-term-care hospitals.
Charles “Chip” Kahn, president of the Federation of American Hospitals, said the greatest immediate impact from the proposal would be the sharp increase in federal money to help cover the cost of treating patients without means to pay their bills. “It is a recognition of what appears to be a trend in uninsured patients across the country,” Kahn said. “It is critically important to hospitals.”
In pressing for more consumer information about prices and better electronic health records, Kahn said, “they’ve got the right direction.”
The American Hospital Association also praised the agency’s steps to “deliver on its promise to ease regulatory barriers.”
Send questions/comments to the editors.


Success. Please wait for the page to reload. If the page does not reload within 5 seconds, please refresh the page.
Enter your email and password to access comments.
Hi, to comment on stories you must . This profile is in addition to your subscription and website login.
Already have a commenting profile? .
Invalid username/password.
Please check your email to confirm and complete your registration.
Only subscribers are eligible to post comments. Please subscribe or login first for digital access. Here’s why.
Use the form below to reset your password. When you've submitted your account email, we will send an email with a reset code.