While states such as Massachusetts and California are grappling with issues of hospital overcrowding, Maine has the opposite problem.
The bulk of Maine’s hospitals are below the national average for occupancy rates, which raises questions about whether the state needs all 36 of its acute care centers.
Hospital officials, however, said the number of beds filled is not a complete gauge of hospital effectiveness.
With advances in technology, hospitals are performing more outpatient procedures intended to keep people from having to check into hospitals for care in the first place.
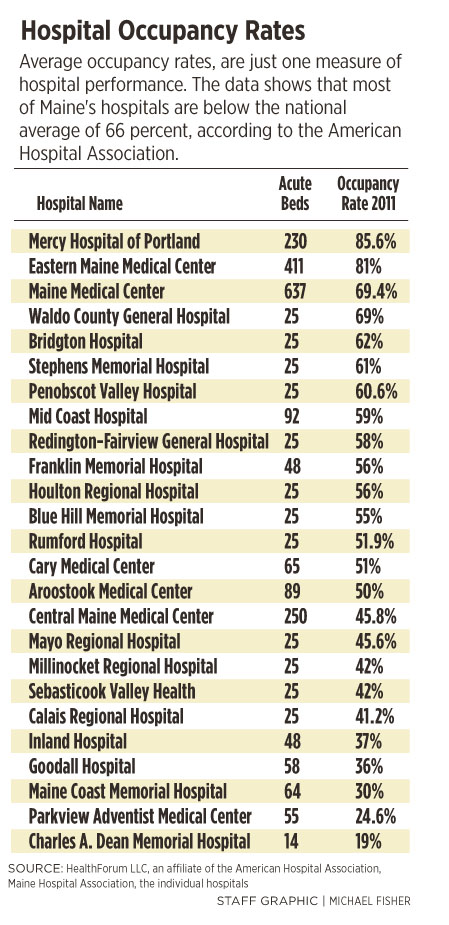
The issue is timely, with the ongoing battle over Parkview Adventist Medical Center in Brunswick, which had an average occupancy rate of 24.6 percent for its 55 beds in 2011. That compares to the national average of 66 percent, according to the American Hospital Association.
Parkview Adventist’s rival, Mid Coast Hospital, wants to combine the two hospitals, eliminate duplicated services and save an estimated $24.3 million a year.
Central Maine Healthcare, which is also bidding to acquire Parkview, wants to keep Parkview Adventist operating and add it to its network, which includes Central Maine Medical Center, Rumford Hospital and Bridgton Hospital.
“It’s pretty expensive to keep beds open,” said Eugene Litvak, president and chief executive of the Institute for Healthcare Optimization in Massachusetts, a nonprofit organization focused on decreasing the cost of health care and improving its quality.
According to Litvak, who is also an adjunct professor at the Harvard School of Public Health, Parkview Adventist’s 24.6 percent occupancy rate “is a huge, huge waste. You’d have to either fill up the hospital more or downsize.”
Above: Occupancy rates in Maine hospitals. Dot sizes are proportional to each hospital’s number of beds. Blue dots are hospitals with high occupancy rates; red dots are hospitals with lower occupancy rates.
Among the Maine hospitals that responded to questions about its occupancy rates, Parkview has the second-lowest occupancy rate, according to a review by the Portland Press Herald/Maine Sunday Telegram. Several hospitals did not respond to requests for data.
The only hospital polled with a lower rate of occupancy is Charles A. Dean Memorial Hospital in Greenville, one of 16 hospitals in Maine in the Critical Access Hospital (CAH) Program.
That designation means the hospital receives special cost-based reimbursement from Medicare, which is extended to small, rural hospitals to help them financially and reduce hospital closures.
Parkview Adventist’s President and Chief Executive Randee Reynolds said the hospital hopes to benefit from Central Maine’s administrative services, technology and research to help reduce its costs.
Reynolds said that while Parkview Adventist may need to better market its services to fill more beds, he stressed that hospitals make more money on surgeries and diagnostics tests than filling hospital beds.
“We have to go out in the community and market our services a little better. Sometimes we don’t tell our stories very well,” Reynolds said. “Where we’re heading in society, though, is how many people you keep out of the hospital, rather than filling the hospital.”
Parkview has rebuffed the partnership proposed by Mid Coast, and officials said they never considered partnering with the crosstown rival.
The state Department of Health and Human Services is set to examine Central Maine’s proposal to acquire Parkview and the plan’s effect on total health care expenditures, the competing demands in the area and whether less costly alternatives are available.
At the other end of the spectrum, Eastern Maine Medical Center in Bangor, Mercy Hospital of Portland and Maine Medical Center, also in Portland, had the highest occupancy rates of the hospitals that responded to questions.
Certain factors affect the average occupancy rates at hospitals, which have been falling nationally in recent decades as technology improves, patients spend less time in the hospital and more procedures are done on an outpatient basis.
Changes in insurance reimbursement also have put pressure on hospitals to cut costs and reduce the length of a patient’s stay.
“There are competing risks. Extremely high occupancy rates cause problems of overcrowding and back-ups in emergency departments if there’s not room for admissions. Too low is problematic because the revenue is too low to keep the hospital functioning. There’s probably a sweet spot in the middle,” said Dr. Karen Joynt, a health policy researcher with the Harvard School of Public Health.
A higher occupancy rate does not automatically mean a hospital is better off financially.
Many issues come into play, ranging from proper staffing for the number of occupied beds on any given day, to the severity of the cases, to the type of reimbursement or payment received, to the amount of charity care provided.
“Individuals can’t live without a paycheck. Hospitals can’t survive without filling beds,” Litvak said. “There’s no answer to the question of optimal occupancy. Overcrowding is bad but under-utilization raises other questions.”
Erik Steele, chief medical officer at Eastern Maine Healthcare Systems, said some small or regional hospitals have scaled back certain services because they may not have the staff to handle complex health problems, and have focused instead on a core group of procedures.
“The low-volume issue has an impact, but it’s hard to quantify,” Steele said. “It’s certainly true as the numbers of patients you have with certain complex problems gets small, you have trouble preventing against skill-set degradation. Not every organization is comfortable with every problem.”
The most complex cases are sent to bigger urban hospitals in Bangor, Portland or even Boston, where there is a diversity of staff and expertise, and more experience handling unusual or complex problems.
While too few occupied beds is a risk, hospitals also face financial problems when they are too full or overcrowded. More mistakes are made, infection rates rise, more patients die and readmission rates increase, experts said.
Hospital officials said occupancy rates are only one metric for rating hospitals.
As more care shifts to outpatient clinics, rehabilitation services and home health services, hospitals are becoming a smaller and smaller piece of the overall medical system.
“Beds is less of a marker of what hospitals are doing these days,” Steele said.
While Litvak said occupancy rates could rise under the Affordable Care Act, as more people get access to health insurance, others suggest that the swing towards outpatient care will be more likely to increase.
The battle over Parkview is just one of several changes afoot in Maine’s health care system.
The parent of Mercy Hospital signed a letter of intent to be acquired by Eastern Maine Healthcare, the parent of Eastern Maine Medical Center.
Goodall Hospital in Sanford recently got approval to join MaineHealth, which includes Maine Medical Center in Portland and 10 other hospitals.
Staff Writer Jessica Hall can be contacted at 791-6316 or at:
jhall@mainetoday.com
CORRECTION: This story was updated Dec. 18, 2012 to reflect that Erik Steele’s title is chief medical officer of Eastern Maine Healthcare Systems, not Eastern Maine Medical Center.
Send questions/comments to the editors.


Success. Please wait for the page to reload. If the page does not reload within 5 seconds, please refresh the page.
Enter your email and password to access comments.
Hi, to comment on stories you must . This profile is in addition to your subscription and website login.
Already have a commenting profile? .
Invalid username/password.
Please check your email to confirm and complete your registration.
Only subscribers are eligible to post comments. Please subscribe or login first for digital access. Here’s why.
Use the form below to reset your password. When you've submitted your account email, we will send an email with a reset code.