AUGUSTA — Doctors, researchers and recovering addicts showed up in force Thursday to oppose the LePage administration’s proposal to eliminate methadone as a reimbursable MaineCare benefit.
More than a dozen medical professionals countered the administration’s stance that Suboxone could replace methadone treatment, pointing out that research shows they are different medications and in many cases serve separate populations of addicts.
Those who suffer from more severe opiate addictions often are not good candidates for Suboxone, but can be treated with methadone, doctors said.
“I prescribe Suboxone on a daily basis, and I believe that it is an excellent medication,” said Dr. David Moltz, a Brunswick doctor, and one of many who testified before a joint meeting of the Appropriations and the Health and Human Services committees Thursday. “However, I am deeply opposed to eliminating methadone as a treatment option. The drugs are not the same, and both are needed for effective treatment of opioid addiction.”
But Health and Human Services Commissioner Mary Mayhew said Suboxone can be prescribed by a family doctor as a take-home medication, while methadone, by law, must be dispensed at a clinic when it is used to treat addiction.
“We believe in an integrated approach to treatment in a primary care setting,” Mayhew said.
Former Republican state representative Kathleen Chase, of Wells, submitted written testimony supporting the administration, calling Suboxone a “true” recovery program, while she claims methadone enables continued addiction.
“(With Suboxone) you walk in taking addicting drugs and walk out not taking addicting drugs,” Chase said in a statement.
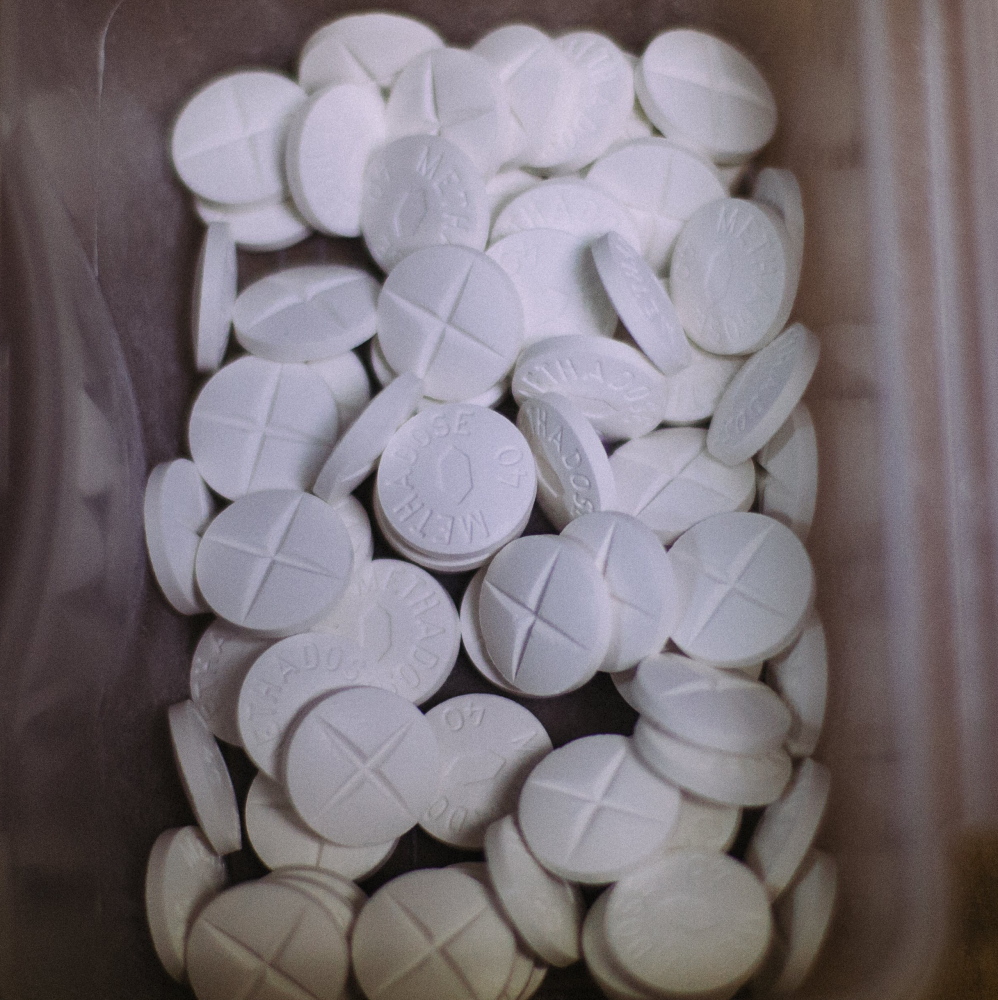
About 4,000 MaineCare patients are treated at 11 methadone clinics. While they could continue receiving methadone treatments by paying out-of-pocket, the $90-$100 cost per week is prohibitive for low-income Mainers who qualify for MaineCare. That’s what Maine calls Medicaid, the program that is administered by the state and funded with federal and state dollars.
Opioid treatments are an optional benefit under Medicaid, so states have the flexibility to cover the treatments, or not. Seventeen states currently do not reimburse for methadone treatments, according to the administration.
A Feb. 20 letter signed by representatives of the American Psychiatric Association, American Society of Addiction Medicine, Northern New England Society of Addiction Medicine and three other medical groups urged Mayhew to continue MaineCare reimbursements for methadone.
“I do not know of an addiction specialist or provider who supports what you are proposing, and at this point I fear this is an administrative initiative that is intruding itself into medical judgments and science without grounding in either one,” said Dr. Steve Bien, a Farmington physician.
When pressed by lawmakers for scientific support for the administration’s proposal, Mayhew said she didn’t immediately have the names of Maine doctors or scientists who supported the administration’s view, but she referred to studies that touted the effectiveness of Suboxone, showing that in some cases, it’s superior to methadone.
Although eliminating methadone reimbursements would reduce spending by $800,000 per year, Mayhew acknowledged that there likely would be no net savings because of increased Suboxone reimbursements.
According to a 2012 study published on the U.S. National Institutes of Health website, Suboxone is not as effective for those with severe addictions.
“The proposal to cut methadone and shift patients to Suboxone is not supported by medical practice and scientific evidence,” said Jennifer Minthorn, assistant vice president for Community Substance Abuse Centers in Lewiston and Portland.
A few people told their personal stories of addiction and how methadone helped them recover.
“Perhaps the only person who receives more shame and stigma than a drug addict is someone who goes to a methadone clinic for help. We would rather point our fingers and blame than see the truth,” said Bruce Campbell, who described himself as being in “long-term recovery” and representing the Bangor Area Recovery Network.
The proposal will go before the health and human services committee for further review in the coming weeks.
Copy the Story LinkSend questions/comments to the editors.



Success. Please wait for the page to reload. If the page does not reload within 5 seconds, please refresh the page.
Enter your email and password to access comments.
Hi, to comment on stories you must . This profile is in addition to your subscription and website login.
Already have a commenting profile? .
Invalid username/password.
Please check your email to confirm and complete your registration.
Only subscribers are eligible to post comments. Please subscribe or login first for digital access. Here’s why.
Use the form below to reset your password. When you've submitted your account email, we will send an email with a reset code.