BRUNSWICK — Much has been said and continues to be said about our aging population and the challenges they and society face. Nothing is ever said, however, about the problem of persistent, or chronic, pain in this population.
It is estimated at least 50 percent of older adults have persistent pain. In many, it is not recognized, or if it is, the persistent pain is untreated or undertreated, all resulting in harm.
Clouding the picture are prejudice, lack of knowledge and/or inaccurate statements believed by health professionals and the public.
Fear of addiction is prevalent, yet rarely do people become addicted when taking medication for pain. They can become physically dependent; however, that can happen with many other medications as well, such as SSRI antidepressants.
The attitude “You just have to live with it” is common but wrong. Pain can be treated effectively, and the treatment, while not completely removing the pain, can allow for functioning and improved quality of life. No one should have to live with pain. Even the World Health Organization says pain management is a human right.
PAIN NOT JUST A PART OF AGING
There are other myths more specific to pain in the older adult, the most common one being: “Pain is part of getting older.”
We don’t acquire pain just because of aging; however, many diseases associated with aging do cause pain and, as we live longer, we have more time to acquire pain syndromes.
Patients face other barriers as well: stoicism (especially here in Maine); belief in the paternal aspect of medicine (“He is my doctor and he is always right”); fear of judgment by family and caregivers, and financial concerns.
Barriers from the health care providers’ side include lack of education. Neither physicians nor nurses actually get much education on pain in school and very little thereafter unless they seek it out.
The prolonged stress of unrelieved pain can affect the heart, the lungs, the GI system (the gut) and the musculoskeletal system (the ability to walk and move around, leading to increased risk of falling and hindering the ability to exercise).
In older adults, especially, we can see a decline in the ability to do everyday things, depression, decreased appetite, anxiety and an impaired ability to think clearly. Pain can also cause or increase confusion, aggravate illness and lead to death – as we lose the ability to function, we increase the likelihood of dying. Most important of all, persistent pain diminishes quality of life.
Pain syndromes are not one thing. Pain can be caused by many different diseases and syndromes: osteoarthritis; rheumatoid arthritis; gout; narrowing (stenosis) of the spinal cord; compression fractures of the spine; shingles; trigeminal neuralgia; post-stroke pain; persistent post-operative pain; fractures old and new; peripheral neuropathies; peripheral vascular disease; temporal arteritis; degenerative joint disease, and many more. Even cancer-related pain has many causes, from the cancer itself to treatments used to cure or control the cancer.
As people respond to treatments individually, we need different treatment options. Planning a balanced regimen – including medication and nonmedication interventions, sometimes psychological help such as coping skills – is important for everyone, especially older adults.
Fear of opioids is rampant, yet they are very helpful in managing persistent pain. One reason for the fear is poorly done studies (such as one mentioned in an Oct. 2, 2013, McClatchy Newspapers article, quoting the number of deaths from overdose), as well as articles that confuse addiction with chronic pain (two separate problems).
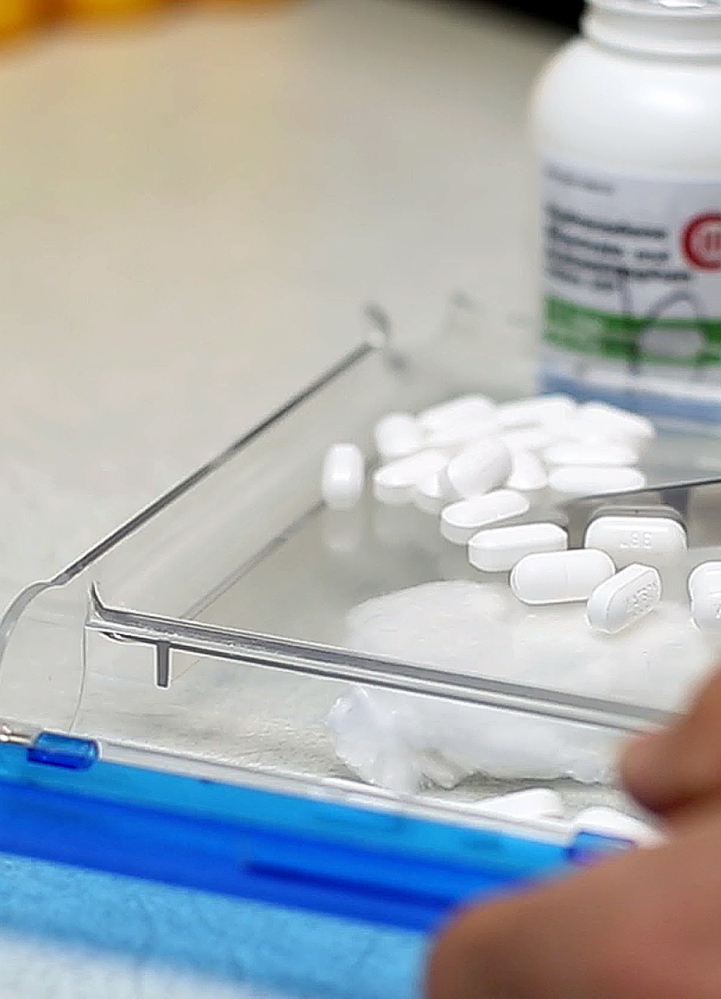
MEDICATION GUIDELINES
Opioids are safe when taken as prescribed – and they need to be prescribed correctly. Side effects of medication need to be managed as well. Other medications, like acetaminophen or tricyclic antidepressants, are sometimes useful in decreasing the amount of opioids needed. Occasionally they can be used instead of opioids. (Nonsteroidal anti-inflammatory drugs, such as ibuprofen, are rarely safe for use in the older adult because of dangerous side effects.)
Important guidelines are available from the American Geriatric Society. Their publication “The Pharmacological Management of Persistent Pain in Older Persons” is written by geriatric experts and is evidence-based.
Nonpharmacological treatments such as massage, guided imagery and acupuncture can be invaluable; however, they’re rarely paid for by insurance. Even those that are covered (such as physical therapy) may not allow sufficient visits. Frequently there isn’t time or availability for coping skills to be taught.
Persistent pain presents many challenges in the older population. However, it is important that they are addressed and not ignored. It is truly a matter of life itself.
— Special to the Telegram
Send questions/comments to the editors.


Comments are no longer available on this story